Top 4 Implementation Science Trends to Watch in 2026
Every year, the healthcare industry works to make patient care smarter, faster and more effective. One way it does this is by translating the latest research into real-world solutions, a process known as implementation science. And just like the healthcare challenges implantation science addresses, trends in this field evolve quickly.
In 2026, staying current with these shifts is essential for anyone working to advance evidence-based practices. From tech-driven tools to equity-focused approaches, here are four trends shaping implementation science this year.
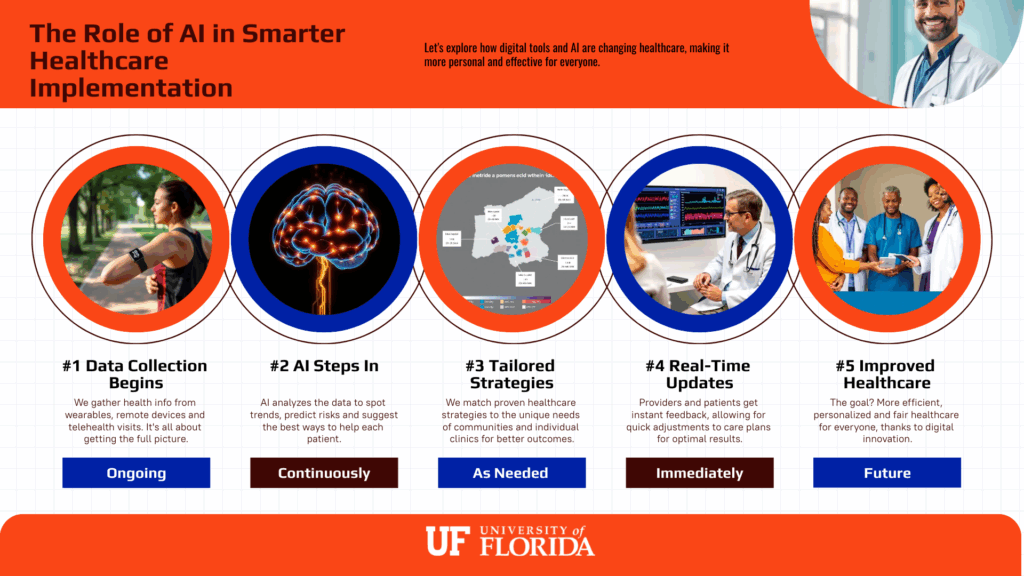
#1 Digital Health and AI
While 2025 was about experimenting with digital tools, 2026 is shaping up to be the year of refining, optimizing and scaling them across different healthcare settings.
One exciting development in implementation science is the increased use of AI-driven tools. Some of these technologies can help predict which interventions are most likely to succeed in specific settings.
The result? More targeted and effective implementation.
For example, an AI system might analyze local clinic data to identify which diabetes prevention programs are most likely to help a rural community. This saves time and resources while improving outcomes.
Other digital health tools play a big role in the industry’s future as well:
- Remote monitoring devices
Provider-facing tools like digital blood pressure cuffs or connected weight scales track vital signs and share data in real time. This helps care teams adjust treatment before problems escalate. - Wearable sensors
Patient-facing devices like fitness watches, glucose monitors or smart rings capture daily health behaviors and outcomes. They make it easier to personalize care plans. - Telehealth platforms
Virtual care systems connect providers and patients, no matter how far apart they are. With these tools, communities with fewer healthcare resources now have more access to reliable care.
Together, these technologies allow for quick adjustments and more efficient, impactful implementation of evidence-based practices. For professionals in the field, this means that digital health is no longer optional — it’s an essential part of supporting diverse patient populations.
#2 Health Equity and Community Engagement
A major theme from 2025 continues into 2026: making sure implementation science supports all patients, not just those with the best access to care. The focus this year will likely include turning equity from a discussion into measurable action.
A big part of this push will depend on community engagement. When community members are involved in planning and carrying out interventions, the results are more likely to be effective and trusted. This approach makes sure that each intervention’s strategies reflect cultural values, social needs and real-life barriers.
For instance, a local clinic might work with community leaders to adapt a diabetes prevention program so it fits cultural practices and daily routines, boosting participation and trust.
Key focus areas in 2026 include:
- Cultural tailoring: Designing programs that reflect the traditions and values of the communities they serve
- Community partnerships: Working directly with local leaders and organizations to improve trust
- Equity as a core goal: Making fairness and access central to every stage of implementation
By centering equity and inclusion, implementation science can deliver stronger, longer-lasting results that reach those who need them most.
#3 Flexible and Adaptive Implementation Models
Healthcare is fast-paced and evolving, and strategies from five or 10 years ago don’t always hold up. In 2026, there will likely be a stronger push for flexible approaches that can adjust to different settings and evolving needs.
Some focus areas may include:
- Testing and learning quickly: Trying out smaller pilot programs and scaling up what works
- Adapting to local needs: Customizing interventions for specific communities or care environments
- Using feedback loops: Collecting data in real time and making changes on the fly
By leaning into adaptability, implementation science can respond faster to challenges and keep pace with new discoveries.
#4 Education and Professional Development
As implementation science grows, so does the need for professionals who understand how to put research into practice. In 2026, more programs are being created to give researchers, clinicians and public health workers the tools they need to make evidence-based interventions work.
These opportunities are becoming easier to access, ranging from short workshops to full certificate programs. The emphasis is on real-world skills: things professionals can take back to their workplaces and apply right away.
Examples of professional development in 2026 include:
- Workshops and seminars focused on practical problem-solving
- Graduate-level certificates that provide a deeper understanding of implementation methods
- Online learning options that make training more flexible and accessible
Investing in professional growth allows individuals to stay ahead of the curve and help lead meaningful change in healthcare and public health.
Frequently Asked Questions About Implementation Science
Implementation science is still a new concept for many people, and it can feel like a dizzying mix of research, healthcare and public health all rolled into one. To clear things up, here are some common questions readers often have about the field — and what the answers mean for 2026 and beyond.
- What is implementation science in simple terms?
Implementation science is about figuring out the best ways to take research findings and put them into real-world practice. Instead of asking, “Does this treatment work?” it asks, “How can we make it work for patients in everyday healthcare settings?” - Why is implementation science important in 2026?
Healthcare is changing fast — from new technologies to growing patient needs. Implementation science makes sure evidence-based practices don’t just sit in research journals but actually improve care in clinics, hospitals and communities. - How does AI fit into implementation science?
AI can help predict which programs will work best in certain settings. For example, it might analyze data from a rural clinic to recommend the most effective diabetes prevention program for that specific community. - What career opportunities are there in implementation science?
Professionals in this field may work as researchers, program evaluators, healthcare administrators or public health specialists. Many roles involve designing, testing and scaling evidence-based interventions across different healthcare settings.
Stay Ahead and Make a Difference
2026 is shaping up to be a year of big changes in implementation science. Some are powered by AI, others are focused on people and communities. By keeping up with these trends, you can make sure that evidence-based interventions truly make a difference in healthcare and public health.
Want to dive deeper? The University of Florida’s entirely online Graduate Certificate in Implementation Science makes it easy to learn on your schedule. In under a year, you can:
- Explore top frameworks
- Discover how to involve diverse communities in your projects
- Master strategies to bring cutting-edge medical innovations into real-world practice
Curious? Check it out and see how you can start making an impact.
Other articles you may be interested in:
- Preventing Hospital Readmissions with Implementation Science
- Implementing Change: 4 Ways Technology Is Revolutionizing Implementation Science
- 5 Ways to Create Mental Health Initiatives That Work
- Top 4 Implementation Science Trends to Watch in 2026
- Cracking the Code: Implementation Science and Epigenetics in Healthcare

